The Dangerous Stigmas Around Mental Health

By Adam A Meyers
The issue of mental health is prominent everywhere in the public safety profession and it is an issue that commands a new perspective.
My name is Adam A. Meyers and I was a Police Officer in Wisconsin – USA for 21 years. In April 2016, I was involved in a critical incident when I used deadly force against someone who armed themselves with a hatchet inside a busy department store. This person died.
I faced many personal and professional mental health challenges after my critical incident and it has taken me many years to get back on track. I would not have been successful with my mental health without the unwavering support of my family, friends, colleagues, and even strangers.
The issue of mental health is prominent everywhere in the public safety profession and it is an issue that commands a new perspective.
So what is Stigma? According to the Webster’s New World Dictionary, the definition of Stigma is, “a mark of disgrace or reproach.” Public safety professionals who struggle with mental health issues often feel devalued and fearful because of the negative attitude society and others in their profession may have against them. As a result, public safety professionals struggling with mental health issues may not get the help they need for fear they’ll be discriminated against, or even worse, terminated.
The public safety profession is a high stress environment that has been closely associated with mental health issues. Public safety professionals who openly seek help for anxiety, depression, emotional disorders, or post-traumatic stress often face personal or professional criticism, discrimination, and sometimes termination. This should not deter them from seeking help, but it does. We need to work together to stop the stigma.
Public safety professionals may choose to treat their mental health issues with poor coping strategies such as excessive consumption of alcohol, drug abuse, casual sex, and other risky behavior. These strategies are self-destructive and tend to cause more stress, anxiety, and depression. They may also become criminal. Below are some of the ways that I used coping strategies negatively. The following may be triggers to those of you who have coped in similar ways.
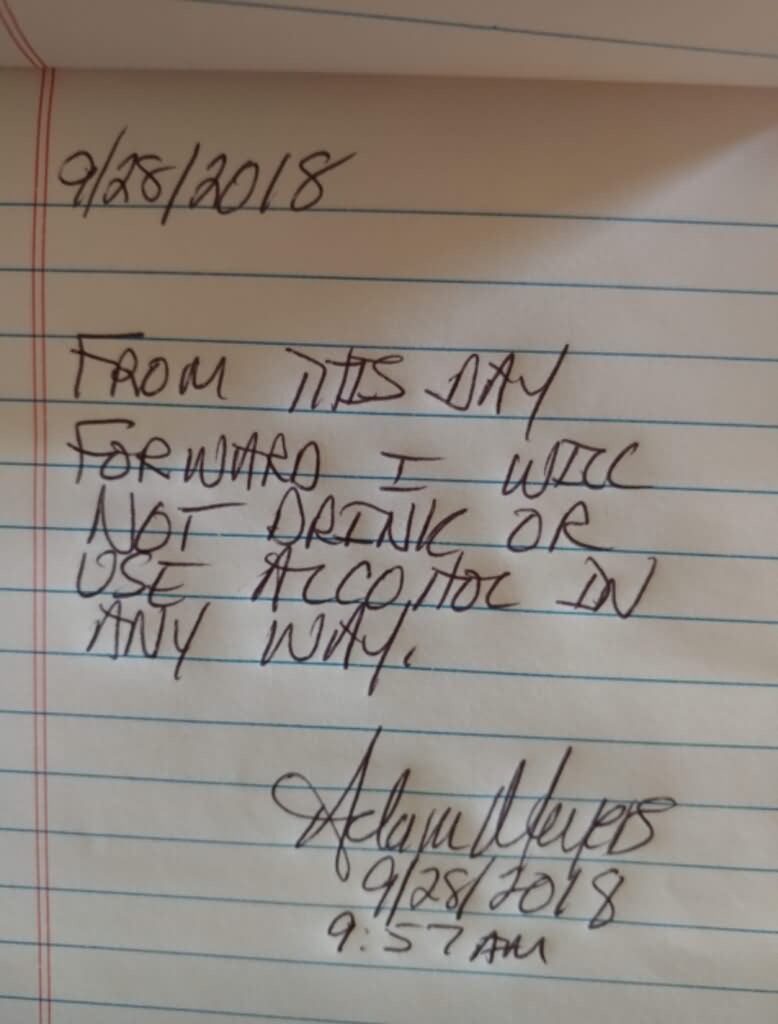
One of my many poor coping strategies was abusing alcohol. Prior to my critical incident I collected wine and enjoyed a glass of wine every now and then. However, after my critical incident I began abusing liquor, mainly whiskey and the cheapest vodka I could get my hands on. I would consume whiskey and vodka straight from their bottles, on the rocks, or I’d create my own cocktails by combining over the counter liquid sleeping or liquid allergy medicines. There were times that I would mix in whatever leftover prescription medicines I had in the medicine cabinet, and it didn’t matter if they were prescribed to me or someone else.
I remember one instance when my oldest daughter had leftover prescribed liquid cough medicine containing codeine. I combined whatever was remining in the bottle with a glass of wine. I was on a prescribed anti-depressant called Venlafaxine while I was abusing alcohol. The label on this medication specially stated, “DO NOT DRINK ALCOHOLIC BEVERAGES WHILE TAKING THIS MEDICATION.” A warning label did not deter me from abusing alcohol. I very well could have blacked out and never woken up from consuming these dangerous cocktails, but at the time I didn’t care. I wanted an escape from my emotional pain. Abusing alcohol may have been a quick fix, but it caused me even more stress, anxiety, and depression.
Another way I dangerously coped was drinking and driving. Prior to attending any type of social event, even as simple as going to the grocery store, I would consume alcohol. I would travel to a nearby gas station and purchase many small bottles of liquor containing about 1.5 ounces of whiskey, vodka or whatever I could afford at the time. I would immediately consume the alcohol in my vehicle prior to travelling to my destination. I tossed the empty bottles in the back of my vehicle or out the window while I was driving. I would rationalize that it would take about 30 minutes for me to feel the effects of the alcohol and by the time I was impaired I would have arrived at my destination. I was very fortunate that I was not arrested for drinking and driving or even worse, killing someone.

My duty weapon during my critical incident was a Glock 22 Gen 4 – 40 Caliber. I put my duty weapon to my head at least a dozen times. Sometimes I even placed the barrel in my mouth. I would always remove the magazine, but for those of you who are not familiar with a Glock, if you don’t rack the slide and remove the round from the chamber (barrel) it will still discharge a round. I very easily could have accidentally killed myself. My rationalization was that I simply wanted to hear and feel the metallic click of the trigger being pulled while the barrel of the gun was resting against my right temple. I did this while I was under the influence of alcohol. I still don’t truly understand why I did this and sometimes wonder how many times it happened while I was blacked out from excessively consuming alcohol. I’m very fortunate to be alive.
I used casual sex to distract myself from my emotional discomfort and pain. I would meet women and sometimes within 30 minutes we would have sex. This caused me more stress and anxiety than anything else. Sure, I felt great during sex, but it caused me more harm than good. Although this type of sexual behavior was risky, self-destructive, and caused me stress and anxiety, it wasn’t enough to convince me to stop. I wanted an instant feel-good escape from my life and casual sex provided that for me.
To overcome the mental health stigma in the public safety profession it is important that those public safety professionals who suffer from mental health issues learn to understand, accept, and determine what is needed to treat it. It is time to become a part of the solution and work with those suffering to make mental health issues stigma free.
Public safety leaders must take a helpful approach when anyone in their command is struggling from mental health issues. Leaders should establish peer support groups and actively participate in them. Leaders, “Are you a part of the problem or the solution?”
Public safety professionals need to be able to trust the leaders and colleagues of their departments to recognize the obstacles and stigmas associated with mental health. They need to feel comfortable and confident that if they are involved in a critical incident and later struggle with mental health issues from the incident, that help will be available with no strings attached.
Remember, mental illness is a medical disorder and not a character flaw or a sign of personal or professional weakness.
https://www.stopthethreatstopthestigma.org/
Podcast
Contests & Promotions